|
Case Report
Fracture of an osseointegrated dental implant in an implant-supported mandibular overdenture
1 DMD, Zobozdravstvo Diamant, Opekarniška cesta 15D, 3000 Celje, Slovenia
2 MD, DMD, PhD, Associate Professor of Oral and Maxillofacial Surgery, OMF kirurgija, Kidričeva 24, 3000 Celje, Slovenia
Address correspondence to:
Marko Božič
MD, DMD, PhD, OMF kirurgija, Kidričeva ulica 24, 3000 Celje,
Slovenia
Message to Corresponding Author
Article ID: 100037Z07JK2021
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Kavčič J, Božič M. Fracture of an osseointegrated dental implant in an implant-supported mandibular overdenture. J Case Rep Images Dent 2021;7:100037Z07JK2021.ABSTRACT
Introduction: Implant fracture is a rare late biomechanical complication with incidence between 0.2% and 1.5%. Factors which may lead to this complication are irregularities in the design and material of the implant, prosthetic superstructure which is not passively connected to the implant and overload. Loosening of prosthetic superstructure, screw fracture, marginal bone loss and peri-implant inflammation are warning signs of implant fracture. Treatment alternatives are removal of the fractured implant, removal of the coronal part of the fractured implant with a new prosthetic post-placement into the remaining integrated part or just conservation of the remaining integrated part of the implant without post placement.
Case Report: A case report about a fracture of the abutment screw and later of an implant fracture and implant removal of the same patient will be presented.
Conclusion: Due to a growing number of patients receiving treatment with dental implants, the risk factors of dental implant fractures must be considered no matter which implant system is used and higher absolute numbers of fractures can be expected.
Keywords: Complication, Fracture, Implant, Overdenture
Introduction
Treatment of complete edentulism with the use of dental implants has been used as a highly successful treatment modality in the last decades. However, with the growing popularity of this kind of treatment, the likelihood of complications associated with dental implants has also increased [1],[2],[3]. Fracture of osseointegrated dental implant is a rare complication which presents a frustrating problem for both the clinician and the patient. Estimated incidence of this late biomechanical complication is between 0.2% and 1.5% [4],[5]. Clinically fracture of the implant can manifest as increased mobility of the prosthetic superstructure, increased pocket depth, and increased gingival indexes of the affected implant. Plaque accumulation is also common because patients are afraid of pain and bleeding when they are brushing their teeth. Radiological assessment can reveal separation of the implant and signs of bone loss [5]. The three main groups of factors leading to this complication are failure in implant design and material, non-passive fitting of the crown of the prosthetic superstructure and overloading secondary to parafunctional habits [6]. Loosening of abutments or screw fractures, marginal bone loss, and peri-implant inflammation are all warning signs which occur before implant fracture in 59% of the cases [7]. Sánchez-Pérez et al. [5] presented risk factors for implant fracture which they divided into three groups related to the patient (pocket depth more than 5 mm, bone loss, overload), implant (diameter less than 4 mm, crown/implant ratio more than 1, implants design), and prosthesis (loosening or torsion of the prosthesis screw, cantilevers, ceramic fracture). They suggest that in the presence of more than three factors, the risk of fracture is high. Treatment of the fractured implant can be either with complete removal of the implant, removal of the coronal part of the fractured implant with a new prosthetic post-placement into the remaining integrated part or just conservation of the remaining integrated part of the implant without post-placement [6],[8]. The first option is usually the treatment of choice. Kits for removal and retrieval of screw fragment, abutment and implant are provided by several companies. Trephine bur or thin surgical bur is used for this purpose to remove the bone surrounding the fractured implant which is then completely removed using forceps [9]. A case of a male patient with a fractured implant which supported a Locator (Astra Tech, Dentsply, Sweden) retained mandibular overdenture will be presented and the possible causes of fracture will be discussed in this article.
Case Report
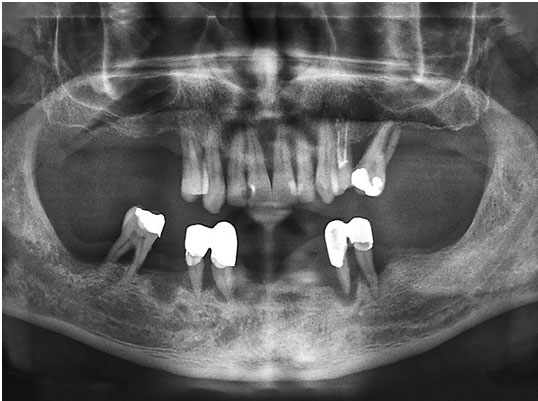
A 57-year-old male visited a maxillofacial surgeon for evaluation of possible treatment with implant supported prosthesis in the upper and lower jaw. The patient was healthy with no significant personal or family medical history. In the maxilla clinical and radiographic examination revealed that teeth from 14 to 24 were present. A few periodontal pockets deeper than 5 mm were present but otherwise the teeth were firm. Tooth 26 was positioned mesially with class 2 mobility (Miller’s classification) and had roots completely exposed. Tooth 24 was endodontically treated with no signs of pain or periapical radiolucency. In the mandible the teeth 33, 34, 43, and 44 presented with class 3 mobility (Miller’s classification). Tooth 46 had exposed bifurcation (Figure 1). The patient was diagnosed with chronic generalized periodontitis. A treatment plan was made which was then presented to the patient. Instructions of proper oral hygiene to avoid teeth and gum diseases were first given to the patient. In the upper jaw conservation of teeth from 14 to 24 and removal of tooth 26 was proposed to the patient. The remaining teeth would undergo scaling and root planing procedure and flap surgery if needed. After periodontal treatment we proposed to replace the missing teeth with implant supported bridge on both sides of the maxilla. In the lower jaw due to poor prognosis removal of all teeth was proposed. An implant supported overdenture was advised to replace the missing teeth in the mandible. All other treatment options, their pros and cons, and financial costs were also discussed. The patient agreed with our proposed treatment plan of the lower jaw which was his primary concern due to the lack of function and aesthetics. However, he decided for a partial removable denture in the upper jaw. An overdenture supported by two implants and retained by a customized bar with built-in retention system was the treatment of choice for the lower jaw. On the day of surgery inferior alveolar block and infiltration anesthesia (Ubistesin Forte, 3M Deutschland, GmbH, Neuss, Germany, 40 mg of articaine chloride per 1 mL, 0.012 mg epinephrine per 1 mL) were first applied to allow for a painless removal of the remaining mandibular teeth and tooth 26. Crestal incision was performed in the interforaminal region. Minimal mucoperiosteal flap was raised followed by excision of excessive granulation tissue of the extraction sockets. The implant sites were prepared in accordance with the manufacturer’s guidelines for Astra Tech Implant System (Dentsply, Sweden). Two implants (Astra Tech, Osseospeed TX 3.5 × 11 and 3.5 × 13 mm, Dentsply, Sweden) were placed obtaining a good primary stability (Figure 2). The patient was instructed to take 1 g of amoxicillin with clavulanic acid (875 mg of amoxicillin/125 mg clavulanic acid) every 12 hours five days postoperatively and to rinse twice daily with 0.12% chlorhexidine solution for two weeks. A soft diet and good oral hygiene were advised. For postoperative pain prevention, non-steroidal-anti-inflammatory drugs were prescribed. Five to seven days of absence from work was also recommended. After two months of osseointegration period of the implants an overdenture retained by a customized cast bar was made by the dentist using the Profile Bar System (Astra Tech, Dentsply, Sweden) (Figure 3). On the regular control visits after the implants placement and overdenture installation the patient had no complaints except occasional abutment screw loosening which was managed by the dentist. Three years after treatment the patient returned to our office with chief complaint of bar mobility. UniAbutment (Astra Tech, Dentsply, Sweden) which was retaining the customized bar on the implant placed in the region 33 fractured. The apical portion of the fractured UniAbutment was also seen on the radiograph (Figure 4). Under local anesthesia (Ubistesin Forte, 3M Deutschland, GmbH, Neuss, Germany, 40 mg of articaine chloride per 1 mL, 0.012 mg epinephrine per 1 mL) a minimal mucoperiosteal flap was raised in the region 33. Approximately 3 mm of bone resorption was seen on the lingual side of the implant. Granulation tissue was removed, and the exposed implant threads were smoothened using a diamond bur. The apical fragment of the UniAbutment was removed using the guiding cylinder and fragment fork of the Astra Tech Implant System removal and retrieval kit. To reduce the stress induced with the customized bar on the supporting implants and to avoid future complications an alternative retention of the overdenture with Locator Abutments (Astra Tech, Dentsply, Sweden) were advised to the patient. UniAbutments were replaced with Locator Abutments which were tightened with the recommended torque of 25 Ncm. The existing overdenture was then modified accordingly. One year later the patient returned to our office with a chief complaint of abutment mobility. Locator Abutment fractured along with the upper part of the implant placed in region 33. A local radiograph was made which confirmed the apical portion of Locator Abutment in the implant (Figure 5) and progression of bone resorption in the occlusal part of the implant. We explained to the patient that the fractured implant has to be removed and replaced with a new implant. We also advised to the patient that if we want to minimize lever forces, which were probably causing these complications, two additional implants in regions 36 and 46 of the mandible have to be placed. The patient agreed with the proposed treatment plan. Mandibular block anesthesia (Ubistesin Forte, 3M Deutschland, GmbH, Neuss, Germany, 40 mg of articaine chloride per 1 mL, 0.012 mg epinephrine per 1 mL) was applied on both sides of the mandible. A crestal incision was performed in region 33 and a minimal mucoperiosteal flap was raised (Figure 6). Fractured implant was seen on the lingual side. Approximately 5 mm of bone resorption was present around the fractured portion of the implant (Figure 7). Appropriate trephine bur was selected from the Astra Removal and Retrieval kit (Astra Tech, Dentsply, Sweden) to remove the surrounding bone of the implant, which was then completely removed using forceps (Figure 8 and Figure 9). A new implant (Astra Tech, Osseospeed TX 3.5 × 11) was then placed in region 32 and two additional implants (Astra Tech, Osseospeed TX 3.5 × 9) in regions 36 and 46 according to the Astra Tech surgical protocol (Figure 10). Existing overdenture was then once again modified to be supported by four implants with Locator Abutments. This kind of treatment minimized lever forces and the possibility of future complications which is to be proven in the future.
Discussion
Treatment of edentulism with complete dentures is still common in Europe. Prevalence of people that are treated with at least one complete denture or a partial removable denture varies between 13% and 29% [10]. However, especially in the mandible, stability and retention problems often occur [11]. Osseointegrated implants introduced new treatment options in the field of removable dentures. By the use of several different retention systems, implant supported overdentures considerably improve function and comfort when compared to traditional removable dentures [12]. When considering the number of implants to be placed to support an overdenture, no difference was found in clinical parameters or patient’s satisfaction between two or four implants. Two implants placed in the interforaminal area are the first treatment option especially when financial constraints are present [13]. Several attachment systems are available in the market which connect an overdenture to the supporting implant. Attachments can either splint the implants or not. When choosing appropriate attachment system to retain an overdenture, factors such as desired level of retention, hygiene, maintenance capability, parallelism of the implants, and financial aspect have to be considered [14],[15]. Bar attachment was our first choice because better retention was desired. Better retention of a bar attachment is also suggested in the literature [16]. However, after the fracture of UniAbutment (Astra Tech, Dentsply, Sweden) occurred, we wanted to reduce the level of stress on the attachment and supporting implants. The physical formula T = F × L (T=torque, F=force, L=length) suggests that when attachment height increases, there will be more lever arm force on the peri-implant bone. This is also supported by the study of Hong et al. [17] who did a finite element analysis on the effect of implant position, angulation, and attachment height on peri-implant bone stress associated with mandibular two-implant overdentures. In this study the authors concluded that to minimize stress the lowest possible height of attachments should be used. Another conclusion of this study was also that to minimize stress on the peri-implant bone, ideally implants should be placed parallel in the mandibular lateral incisor area. Locator abutments (Astra Tech, Dentsply, Sweden) were used in the presented case. These self-aligning attachments maintain vertical and hinge resiliency and are especially useful when interarch distance is inadequate [15]. In the presented case however, Locator abutment also fractured together with the upper part of the implant. The implant had to be removed. Two main causes for late implant fracture are loss of supporting tissue secondary to infection or peri-implantitis and metal fatigue due to mechanical overloading which appears to be the most frequent cause [18]. Inappropriate occlusion as a single factor or combined with bruxism can also cause implant fracture [19]. A recent study by Murakami et al. [20] identified gender, gonial angle, and splinting status of the superstructure as significant risk factors. The study concluded that males, especially those with a mandibular angle of less than 120° on panoramic radiographs, and a non-splinted superstructure present an increased risk of implant fracture. When assessing the risk factors for implant fracture presented by Sánchez-Pérez et al. [5], no history of bruxism was reported by our patient. Due to bone tissue constraints, we did place an implant of diameter under 4 mm but on the other hand some authors suggest that only implants under diameter of 3.5 mm present a risk factor [21]. However, the cantilever factor was present and also loosening of the prosthetic screw did occur in the presented case. Moreover, approximately 3 mm of bone loss was present when the screw of the fractured UniAbutment (Astra Tech, Dentsply, Sweden) was removed. Considering all these factors, more than three risk factors were present which placed our patient in a group with high risk for implant fracture.
Conclusion
In McGill Consensus Statement of 2002 mandibular overdenture retained by two implants is recommended as the first choice for treating mandibular edentulism. Implants connected with various attachment systems to support an overdenture can provide satisfaction of patients and considerably improve their quality of life. Due to a growing number of patients receiving treatment with dental implants, the risk factors of dental implant fractures must be considered no matter which implant system is used and higher absolute numbers of fractures can be expected. The clinicians must plan the treatment carefully. Implant position, angulation, and height of the selected attachment must be taken into account. All the risk factors have to be considered and warning signs must not be overlooked.
REFERENCE
1.
Moraschini V, Poubel LADC, Ferreira VF, Barboza EDSP. Evaluation of survival and success rates of dental implants reported in longitudinal studies with a follow-up period of at least 10 years: A systematic review. Int J Oral Maxillofac Surg 2015;44(3):377–88. [CrossRef]
[Pubmed]

2.
Tey VHS, Phillips R, Tan K. Five-year retrospective study on success, survival and incidence of complications of single crowns supported by dental implants. Clin Oral Implants Res 2017;28(5):620–5. [CrossRef]
[Pubmed]

3.
Gupta S, Gupta H, Tandan A. Technical complications of implant-causes and management: A comprehensive review. Natl J Maxillofac Surg 2015;6(1):3–8. [CrossRef]
[Pubmed]

4.
Berglundh T, Persson L, Klinge B. A systematic review of the incidence of biological and technical complications in implant dentistry reported in prospective longitudinal studies of at least 5 years. J Clin Periodontol 2002;29 Suppl 3:197–212. [CrossRef]
[Pubmed]

5.
Sánchez-Pérez A, Moya-Villaescusa MJ, Jornet-Garcia A, Gomez S. Etiology, risk factors and management of implant fractures. Med Oral Patol Oral Cir Bucal 2010;15(3):e504–8. [CrossRef]
[Pubmed]

6.
Balshi TJ. An analysis and management of fractured implants: A clinical report. Int J Oral Maxillofac Implants 1996;11(5):660–6.
[Pubmed]

7.
Rangert B, Krogh PH, Langer B, Van Roekel N. Bending overload and implant fracture: A retrospective clinical analysis. Int J Oral Maxillofac Implants 1995;10(3):326–34.
[Pubmed]

8.
Jemt T. Failures and complications in 391 consecutively inserted fixed prostheses supported by Brånemark implants in edentulous jaws: A study of treatment from the time of prosthesis placement to the first annual checkup. Int J Oral Maxillofac Implants 1991;6(3):270–6.
[Pubmed]

9.
Yu HC, Kim YK. Fractures of implant fixtures: A retroscccpective clinical study. Maxillofac Plast Reconstr Surg 2020;42(1):13. [CrossRef]
[Pubmed]

10.
Zitzmann NU, Hagmann E, Weiger R. What is the prevalence of various types of prosthetic dental restorations in Europe? Clin Oral Implants Res 2007;18 Suppl 3:20-33. [CrossRef]
[Pubmed]

11.
van Waas MA. The influence of psychologic factors on patient satisfaction with complete dentures. J Prosthet Dent 1990;63(5):545–8. [CrossRef]
[Pubmed]

12.
Bakke M, Holm B, Gotfredsen K. Masticatory function and patient satisfaction with implant-supported mandibular overdentures: A prospective 5-year study. Int J Prosthodont 2002;15(6):575–81.
[Pubmed]

13.
Meijer HJA, Raghoebar GM, Batenburg RHK, Visser A, Vissink A. Mandibular overdentures supported by two or four endosseous implants: A 10-year clinical trial. Clin Oral Implants Res 2009;20(7):722–8. [CrossRef]
[Pubmed]

14.
Gulizio MP, Agar JR, Kelly JR, Taylor TD. Effect of implant angulation upon retention of overdenture attachments. J Prosthodont 2005;14(1):3–11. [CrossRef]
[Pubmed]

15.
Alsiyabi AS, Felton DA, Cooper LF. The role of abutment-attachment selection in resolving inadequate interarch distance: A clinical report. J Prosthodont 2005;14(3):184–90. [CrossRef]
[Pubmed]

16.
Naert I, Quirynen M, Hooghe M, van Steenberghe D. A comparative prospective study of splinted and unsplinted Brånemark implants in mandibular overdenture therapy: A preliminary report. J Prosthet Dent 1994;71(5):486–92. [CrossRef]
[Pubmed]

17.
Hong HR, Pae A, Kim Y, Paek J, Kim HS, Kwon KR. Effect of implant position, angulation, and attachment height on peri-implant bone stress associated with mandibular two-implant overdentures: A finite element analysis. Int J Oral Maxillofac Implants 2012;27(5):e69–76.
[Pubmed]

18.
Piattelli A, Scarano A, Piattelli M, Vaia E, Matarasso S. Hollow implants retrieved for fracture: A light and scanning electron microscope analysis of 4 cases. J Periodontol 1998;69(2):185–9. [CrossRef]
[Pubmed]

19.
Stoichkov B, Kirov D. Analysis of the causes of dental implant fracture: A retrospective clinical study. Quintessence Int 2018;49(4):279–86. [CrossRef]
[Pubmed]

20.
Murakami H, Igarashi K, Fuse M, et al. Risk factors for abutment and implant fracture after loading. J Oral Sci 2020;63(1):92–7. [CrossRef]
[Pubmed]

21.
McDermott NE, Chuang SK, Woo VV, Dodson TB. Complications of dental implants: Identification, frequency, and associated risk factors. Int J Oral Maxillofac Implants 2003;18(6):848–55.
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Jakob Kavčič - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Marko Božič - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guaranter of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2021 Jakob Kavčič et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.